Namaste
Well-Known Member
- Relationship to Diabetes
- Type 2
Good afternoon,
I am struggling again. I'm not sure that what is happening is normal - I would be grateful if someone could help.
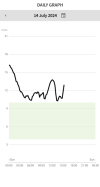
Attached is my sugars from today. I've had very few carbs and no sugary food. It seems that my sugars are spiking about 2-3 hours after I've eaten (and overnight, about 5-6 hours after food). I've been for a walk, but I can't work out what is sending them up. I'm tired and grumpy.
I switched from alogliptin to sitagliptin a couple of weeks ago and at first all was fine, but my sugars have crept up and not staying stable which makes me wonder if the sitagliptin is not working in the way that it should? I do have a review in a fortnight with a nurse so will keep a track, but it's very frustrating. I'm trying very hard to get my HBA1C down again, particularly as I am due surgery and they - rightly - won't do it while my sugar control is not good.
Any help, much appreciated.
Jane
I am struggling again. I'm not sure that what is happening is normal - I would be grateful if someone could help.
Attached is my sugars from today. I've had very few carbs and no sugary food. It seems that my sugars are spiking about 2-3 hours after I've eaten (and overnight, about 5-6 hours after food). I've been for a walk, but I can't work out what is sending them up. I'm tired and grumpy.
I switched from alogliptin to sitagliptin a couple of weeks ago and at first all was fine, but my sugars have crept up and not staying stable which makes me wonder if the sitagliptin is not working in the way that it should? I do have a review in a fortnight with a nurse so will keep a track, but it's very frustrating. I'm trying very hard to get my HBA1C down again, particularly as I am due surgery and they - rightly - won't do it while my sugar control is not good.
Any help, much appreciated.
Jane