Some thoughts: As advertised, remission isn't the end. You can't draw a hand across your brow and exclaim, "I'm glad that's finally over!". I gained back 8.5 lbs with happy eating, and now I'm back on shakes and trying to make my morning sugar behave as per Prof Taylor's instructions when you stray. I knew this was a lifelong commitment, but it's not like the exercise and diet montage with inspirational power cords that went through my head (think, "Rocky"). It's a slog, and it's why so few remain in remission over the long haul. I'm determined to stay in that group, but my evil twin (Malcolm) occasionally takes over my body and does what he will. When he's done it's back to ashes and sackcloth for me. It's worth it though. I read the advice of a doctor that I trust (somewhat) on Youtube. He pointed out that even at an A1c of 5.6 some damage may be occurring. I'll look for more information on that. Now that I'm in the 5's club my next goal will be to get below 5.6. Here endeth the rant.
-
Please Remember: Members are only permitted to share their own experiences. Members are not qualified to give medical advice. Additionally, everyone manages their health differently. Please be respectful of other people's opinions about their own diabetes management.
-
Take a look at our new Type 2 Diabetes Remission section on the Diabetes UK website: https://www.diabetes.org.uk/diabetes-the-basics/type-2-remission
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
The Job of Remission
- Thread starter mhtyler
- Start date
- Status
- This thread is now closed. Please contact Anna DUK, Ieva DUK or everydayupsanddowns if you would like it re-opened.
Drummer
Well-Known Member
- Relationship to Diabetes
- Type 2
I had enough punishment for several lifetimes when trying to follow low calorie diets, so in the nanoseconds after being informed that I had type 2, and was a very bad diabetic I changed to eating a low carb diet and (mentally) erected barriers to anything which did not conform to my new philosophy of 'you aren't the boss of me no more'. Next day I used the diet sheets issued by GPs to light the barbecue.
I have never checked my levels first thing - I experimented with meals to find out what I could eat and stuck to that.
Alteration happened.
If I eat more carbs one day, I reduce the next one or two.
I always have things to eat available, so if I feel the urge to eat I have lots of low carb options and that seems to help in maintaining a fairly steady state.
Perhaps I am lucky in that I really do not feel happy eating lots of carbs, particularly if in high carb foods.
I do once in a while, overdo things as in eating all the strawberries yesterday - but I had not eaten strawberries for almost a month, which is, perhaps, my mistake.
I don't do sackcloth and ashes, nor shakes - after all steak and mushrooms followed by strawberries, cream and a bottle of chilled Moscato d'asti is likely to have the same effect in the long term, so why put oneself to the trouble?
I have never checked my levels first thing - I experimented with meals to find out what I could eat and stuck to that.
Alteration happened.
If I eat more carbs one day, I reduce the next one or two.
I always have things to eat available, so if I feel the urge to eat I have lots of low carb options and that seems to help in maintaining a fairly steady state.
Perhaps I am lucky in that I really do not feel happy eating lots of carbs, particularly if in high carb foods.
I do once in a while, overdo things as in eating all the strawberries yesterday - but I had not eaten strawberries for almost a month, which is, perhaps, my mistake.
I don't do sackcloth and ashes, nor shakes - after all steak and mushrooms followed by strawberries, cream and a bottle of chilled Moscato d'asti is likely to have the same effect in the long term, so why put oneself to the trouble?
AndBreathe
Well-Known Member
- Relationship to Diabetes
- In remission from Type 2
I do think that remission is somewhat overplayed these days. I mean; how many folks do we see rock up, wanting to know what to do because they want to be rid of their diabetes? I may be doing those, often newly diagnosed folks a disservice, but some not, for sure.
Personally, I found it relatively easy to reach remission and have stayed there over 10 years, but from that decade of reading and observing, I know I got lucky, and I remain lucky.
I also know that life isn't predictable and like anything long term, the nuances change over time. Life changes, other conditions crop up, the ability to be as active changes (although, I find activity is the figurative icing on the cake, rather than a fundamental). Those are just examples.
I think striving for improvement is important. I was probably helped by the fact that in late 2013 (diagnosis) and early 2014 (first "normal" A1c) the concept of remission was not at all recognised, and dietary management by reduced carb was often seen as the route to ill-health and the arteries of a centenarian. Times change.
The longer terms impacts of remission may, or may not be helpful in terms of living a long and good life. There really hasn't been much done one it, for LONG term impacts.
The cardiac research unit in Leicester is looking at remission, and initial studies have fertilised several more projects (Yay for PhD students needing research), and the diabetes unit is finally perking it's ears up.
All of that work will take some time to come to fruition and publication, but it's a start.
Personally, I found it relatively easy to reach remission and have stayed there over 10 years, but from that decade of reading and observing, I know I got lucky, and I remain lucky.
I also know that life isn't predictable and like anything long term, the nuances change over time. Life changes, other conditions crop up, the ability to be as active changes (although, I find activity is the figurative icing on the cake, rather than a fundamental). Those are just examples.
I think striving for improvement is important. I was probably helped by the fact that in late 2013 (diagnosis) and early 2014 (first "normal" A1c) the concept of remission was not at all recognised, and dietary management by reduced carb was often seen as the route to ill-health and the arteries of a centenarian. Times change.
The longer terms impacts of remission may, or may not be helpful in terms of living a long and good life. There really hasn't been much done one it, for LONG term impacts.
The cardiac research unit in Leicester is looking at remission, and initial studies have fertilised several more projects (Yay for PhD students needing research), and the diabetes unit is finally perking it's ears up.
All of that work will take some time to come to fruition and publication, but it's a start.
Good to hear the diabetes unit at Leicester is finally perking its ears up.The longer terms impacts of remission may, or may not be helpful in terms of living a long and good life. There really hasn't been much done one it, for LONG term impacts. The cardiac research unit in Leicester is looking at remission, and initial studies have fertilised several more projects (Yay for PhD students needing research), and the diabetes unit is finally perking it's ears up. All of that work will take some time to come to fruition and publication, but it's a start.
Would you be able to outline the aims of the initial studies and projects to come a bit more detail?
Thanks.
"The longer terms impacts of remission may, or may not be helpful in terms of living a long and good life. There really hasn't been much done on it, for LONG term impacts."
The damage from high sugar levels is well enough studied, so the impact of normal sugar is necessarily positive. I am concerned that a non-diabetic level just below 6.5 as shown in Prof. Taylor's study may not have the benefit of truly normal A1c numbers at or below say...5.5.
The damage from high sugar levels is well enough studied, so the impact of normal sugar is necessarily positive. I am concerned that a non-diabetic level just below 6.5 as shown in Prof. Taylor's study may not have the benefit of truly normal A1c numbers at or below say...5.5.
Drummer
Well-Known Member
- Relationship to Diabetes
- Type 2
I wanted to reduce down from a HbA1c of 42 after a couple of tests at that level.
I reduced daily intake from a maximum of 50gm to 40gm of carbs, stuck to that for an entire year, and at the next test, was 42. My individual tests after eating were down a bit, so I was hopeful, but I was experiencing problems with carbs, and the insistence that they were healthy for a very long time before diagnosis and I was about 70 years old by then.
Even with my slightly less strict regime these days my last test was 43.
I'm not intending to be more lenient than at present, but I suspect that HbA1c is not entirely fixed by carb intake - at least in the close to normal ranges.
I reduced daily intake from a maximum of 50gm to 40gm of carbs, stuck to that for an entire year, and at the next test, was 42. My individual tests after eating were down a bit, so I was hopeful, but I was experiencing problems with carbs, and the insistence that they were healthy for a very long time before diagnosis and I was about 70 years old by then.
Even with my slightly less strict regime these days my last test was 43.
I'm not intending to be more lenient than at present, but I suspect that HbA1c is not entirely fixed by carb intake - at least in the close to normal ranges.
Professor Tim Noakes is the expert on carb intolerance. In brief he was a long distance athlete years ago when carbohydrate loading was in vogue. If I recall aright, he says his tolerance level nowadays is down to zero on some days and up to 25g on others. Worth checking out his videos.I wanted to reduce down from a HbA1c of 42 after a couple of tests at that level.
I reduced daily intake from a maximum of 50gm to 40gm of carbs, stuck to that for an entire year, and at the next test, was 42. My individual tests after eating were down a bit, so I was hopeful, but I was experiencing problems with carbs, and the insistence that they were healthy for a very long time before diagnosis and I was about 70 years old by then.
Even with my slightly less strict regime these days my last test was 43.
I'm not intending to be more lenient than at present, but I suspect that HbA1c is not entirely fixed by carb intake - at least in the close to normal ranges.
AndBreathe
Well-Known Member
- Relationship to Diabetes
- In remission from Type 2
Good to hear the diabetes unit at Leicester is finally perking its ears up.
Would you be able to outline the aims of the initial studies and projects to come a bit more detail?
Thanks.
Thed initial study's aims were absolutely nothing to do with remission. They were around heart failure and particularly relating to preserved ventricular ejection fraction versus reduced ventricular ejection fraction. Ventricular ejection fraction is the how much of it's volume the left ventricle pumps with each heartbeat. This was/is for those who have had an historic diagnosis of T2.
The reason a sub- cohort of subjects in remission was added because someone asked a question in a meeting which went something like........ "And what about those in remission? What happens to their heart health?"
Nobody knew, and nor could they make educated guesses, because in their clinical work they were seeing patients already experiencing cardiac issues of one sort or another. Of course, not always related to their T2.
A small sub-cohort were recruited, and the existing study data was mined for patients in remission - whether they knew it or not, and a small study kicked off, which attracted quite a bit of interest, both in UK and further afield.
The is the first paper from this sub-study, but there are plenty more being written.
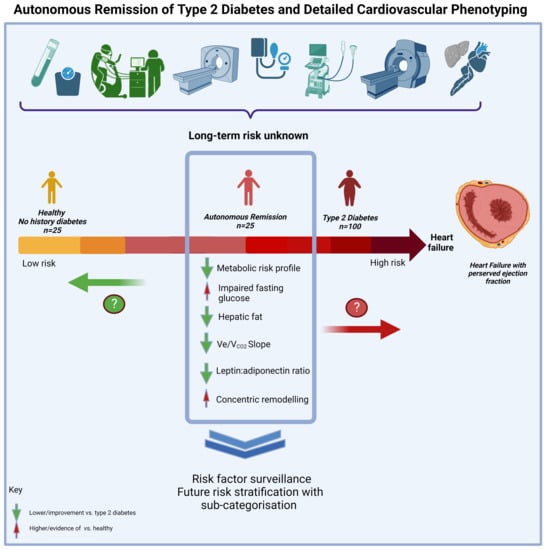
Impact of the Remission of Type 2 Diabetes on Cardiovascular Structure and Function, Exercise Capacity and Risk Profile: A Propensity Matched Analysis
Type 2 diabetes (T2D) confers a high risk of heart failure frequently with evidence of cardiovascular structural and functional abnormalities before symptom onset. The effects of remission of T2D on cardiovascular structure and function are unknown. The impact of the remission of T2D, beyond...
I couldn't find it in the counterbalance study, but I believe Taylor et al accept that a level below 6.5 is non-diabetic. The responders (those who recovered some pancreas function) achieved an average of 6.2 after 6 months on the program. It's an amazing result, but lower is better. The non-responders started out higher, and ended higher. Their pancreas function had only marginal recovery. From the start I appeared to be in a responder category, but I was quite anxious to find out for sure. I know now I am because my response to carbs...even when I'm naughty is something I've never seen before...very glad of that, but I was already determined to finish the course even if I was a non responder. A liver clear of fat is a good thing all by itself.As I recall the criterion for remission in the Counterpoint study was 6.0/42. I found the futher reduction to <5.5/7 was well worthwhile.
Too many papers on the same subject. Anyway the Consensus Report came out in 2021 more than ten years after Counterpoint. Just before that in 2020 Roy Taylor published this interesting review paper in which he discusses inter alia the 'postdiabetic' state between 6.5/48 and 6.0/42: Type 2 diabetes and remission. Getting down to around 5.5/36 is good when possible.I couldn't find it in the counterbalance study, but I believe Taylor et al accept that a level below 6.5 is non-diabetic. The responders (those who recovered some pancreas function) achieved an average of 6.2 after 6 months on the program. It's an amazing result, but lower is better. The non-responders started out higher, and ended higher. Their pancreas function had only marginal recovery. From the start I appeared to be in a responder category, but I was quite anxious to find out for sure. I know now I am because my response to carbs...even when I'm naughty is something I've never seen before...very glad of that, but I was already determined to finish the course even if I was a non responder. A liver clear of fat is a good thing all by itself.
Thank you for this. By coincidence my wife, who is not diabetic, recently had a cardiac event affecting her left ventricle - diagnosed as Takotsubo.Thed initial study's aims were absolutely nothing to do with remission. They were around heart failure and particularly relating to preserved ventricular ejection fraction versus reduced ventricular ejection fraction. Ventricular ejection fraction is the how much of it's volume the left ventricle pumps with each heartbeat. This was/is for those who have had an historic diagnosis of T2.
The reason a sub- cohort of subjects in remission was added because someone asked a question in a meeting which went something like........ "And what about those in remission? What happens to their heart health?"
Nobody knew, and nor could they make educated guesses, because in their clinical work they were seeing patients already experiencing cardiac issues of one sort or another. Of course, not always related to their T2.
A small sub-cohort were recruited, and the existing study data was mined for patients in remission - whether they knew it or not, and a small study kicked off, which attracted quite a bit of interest, both in UK and further afield.
The is the first paper from this sub-study, but there are plenty more being written.
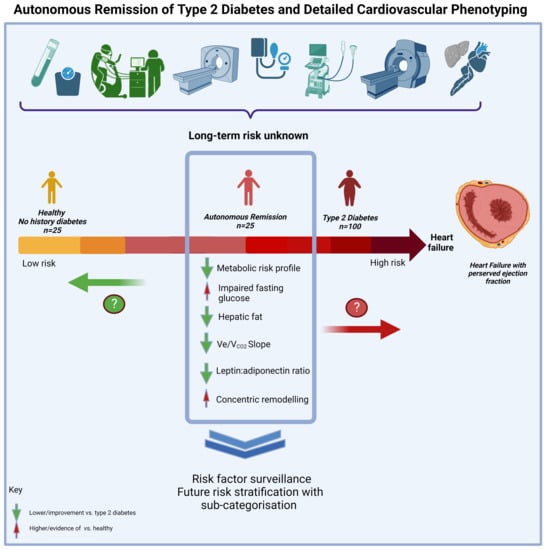
Impact of the Remission of Type 2 Diabetes on Cardiovascular Structure and Function, Exercise Capacity and Risk Profile: A Propensity Matched Analysis
Type 2 diabetes (T2D) confers a high risk of heart failure frequently with evidence of cardiovascular structural and functional abnormalities before symptom onset. The effects of remission of T2D on cardiovascular structure and function are unknown. The impact of the remission of T2D, beyond...www.mdpi.com
At a glance the first paper is very interesting. I'll read it properly shortly. The conclusion abour elevated fasting glucose tallies with Roy Taylor's Counterpoint study. Maybe the next papers will look at the combined effects of fatty liver and T2D.
By the way, I agree with you that achieving remission is not difficult when you choose the right diet, and there are no complications. The problem is the NHS provides no detailed guidance for people to follow when diagnosed. Instead they feel overwhelmed and at sea, in their hundreds of thousands.
AndBreathe
Well-Known Member
- Relationship to Diabetes
- In remission from Type 2
The next papers will still focus on cardiac matters, because the research is being done by the cardiac research unit, and partly funded by the BHF.Thank you for this. By coincidence my wife, who is not diabetic, recently had a cardiac event affecting her left ventricle - diagnosed as Takotsubo.
At a glance the first paper is very interesting. I'll read it properly shortly. The conclusion abour elevated fasting glucose tallies with Roy Taylor's Counterpoint study. Maybe the next papers will look at the combined effects of fatty liver and T2D.
By the way, I agree with you that achieving remission is not difficult when you choose the right diet, and there are no complications. The problem is the NHS provides no detailed guidance for people to follow when diagnosed. Instead they feel overwhelmed and at sea, in their hundreds of thousands.
There is a new piece kicking off shortly that I will know more about after a meeting, shortly. It is still under the cardiac umbrella, but I have a feeling it will have different nuances.
To be fair, the initial paper really just says "more work required", but at least the taste is there, in that unit.
The Leicester Diabetes Centre is where Desmond and Eden emanate from, so diet can be an "interesting" discussion.
Counterbalance*Thank you for this. By coincidence my wife, who is not diabetic, recently had a cardiac event affecting her left ventricle - diagnosed as Takotsubo.
At a glance the first paper is very interesting. I'll read it properly shortly. The conclusion abour elevated fasting glucose tallies with Roy Taylor's Counterpoint study. Maybe the next papers will look at the combined effects of fatty liver and T2D.
By the way, I agree with you that achieving remission is not difficult when you choose the right diet, and there are no complications. The problem is the NHS provides no detailed guidance for people to follow when diagnosed. Instead they feel overwhelmed and at sea, in their hundreds of thousands.
Yes, Counterbalance extending Counterpoint.Counterbalance*
Is there a counterpoint study as well? I've never read that. Where can i find it? thxYes, Counterbalance extending Counterpoint.
Yes, Counterpoint was the original study proving the disorder is reversible in many cases. I'd start with
Prof Taylor's review paper, Banting Memorial Lecture 2012 'Reversing the twin cycles of Type 2 diabetes'. Ther references include some of the papers about the study.
The 2020 article I mentioned earlier is an update with the benefit of ten years hindsight:
Type 2 diabetes and remission: practical management guided by pathophysiology
Prof Taylor's review paper, Banting Memorial Lecture 2012 'Reversing the twin cycles of Type 2 diabetes'. Ther references include some of the papers about the study.
The 2020 article I mentioned earlier is an update with the benefit of ten years hindsight:
Type 2 diabetes and remission: practical management guided by pathophysiology
Docb
Moderator
- Relationship to Diabetes
- Type 2
If I can make an observation....
If only Taylor and Co opened by saying that there are many possible reasons for poor automated blood glucose control other than autoimmune destruction of the cells that produce insulin in the pancreas and these come under the umbrella term of T2 diabetes, then that would help.
What they have shown, and shown convincingly, is that excess fat around the liver and pancreas accounts for poor blood glucose control in a significant number of those with a T2 label and taking measures to reduce that fat in those affected is a very effective method of restoring blood glucose control. They tend to make no reference to those with a T2 diagnosis who are not overweight, indeed if I recall correctly they exclude such people from their studies. The way they report things tends, at least in my view, to make it easy to assume that getting rid of non-T1 diabetes only requires losing a bit of fat. That may be the case for a major subset of those with a T2 diagnosis but does not apply to all.
My take on all this is that if you have a T2 diagnosis and you are overweight then loosing that excess weight offers a very good chance of regaining automatic blood glucose control. I prefer the language of risk and uncertainty rather than the implied positivity in Taylor's (other gurus are available) reporting.
As you might guess I am one of those for whom it does not work. T2 label but not overweight, who's auto blood glucose control would be of concern if I did not take some pills and deliberately control my carbohydrate intake. I accept I am in a minority but I suspect I am far from alone.
If only Taylor and Co opened by saying that there are many possible reasons for poor automated blood glucose control other than autoimmune destruction of the cells that produce insulin in the pancreas and these come under the umbrella term of T2 diabetes, then that would help.
What they have shown, and shown convincingly, is that excess fat around the liver and pancreas accounts for poor blood glucose control in a significant number of those with a T2 label and taking measures to reduce that fat in those affected is a very effective method of restoring blood glucose control. They tend to make no reference to those with a T2 diagnosis who are not overweight, indeed if I recall correctly they exclude such people from their studies. The way they report things tends, at least in my view, to make it easy to assume that getting rid of non-T1 diabetes only requires losing a bit of fat. That may be the case for a major subset of those with a T2 diagnosis but does not apply to all.
My take on all this is that if you have a T2 diagnosis and you are overweight then loosing that excess weight offers a very good chance of regaining automatic blood glucose control. I prefer the language of risk and uncertainty rather than the implied positivity in Taylor's (other gurus are available) reporting.
As you might guess I am one of those for whom it does not work. T2 label but not overweight, who's auto blood glucose control would be of concern if I did not take some pills and deliberately control my carbohydrate intake. I accept I am in a minority but I suspect I am far from alone.
Eddy Edson
Well-Known Member
- Relationship to Diabetes
- In remission from Type 2
No, this is completely untrue & against the whole tenor of Taylor's work. For specifics, check the ReTUNE study.They tend to make no reference to those with a T2 diagnosis who are not overweight, indeed if I recall correctly they exclude such people from their studies.

ReTUNE study shows type 2 remission possible for people with lower body weight
While we know that obesity increases the risk of developing type 2 diabetes, 10% of people with type 2 diabetes have a BMI that is not in the obesity or overweight category.
You seem to be confusing the notion of not having excess visceral fat with the notion of not being "overweight" according to BMI or whatever. If you read the general literature in the field you'll see that visceral fat and related central adiposity have the big health implications & that BMI is useful mainly as a rough & ready proxy for it. This is the reason for NICE et al emphasizing a wasit-to-height ration of <=0.5 as being probably a better health indicator than BMI.
ReTUNE showed the same kind of remission profile with vsiceral fat reduction for BMI-"normal" people, like me, and people with overweight/obesity.
Docb
Moderator
- Relationship to Diabetes
- Type 2
@Eddy Edson ... I stand corrected. Must read the detail. Mind you, I am 66" high with a 32" waist and would still have poor blood glucose control without the pills and watching carbohydrate intake.
- Status
- This thread is now closed. Please contact Anna DUK, Ieva DUK or everydayupsanddowns if you would like it re-opened.
